Cheaper drugs at GP clinics under Healthier SG 'one resident, one doctor' scheme to be launched in 2023
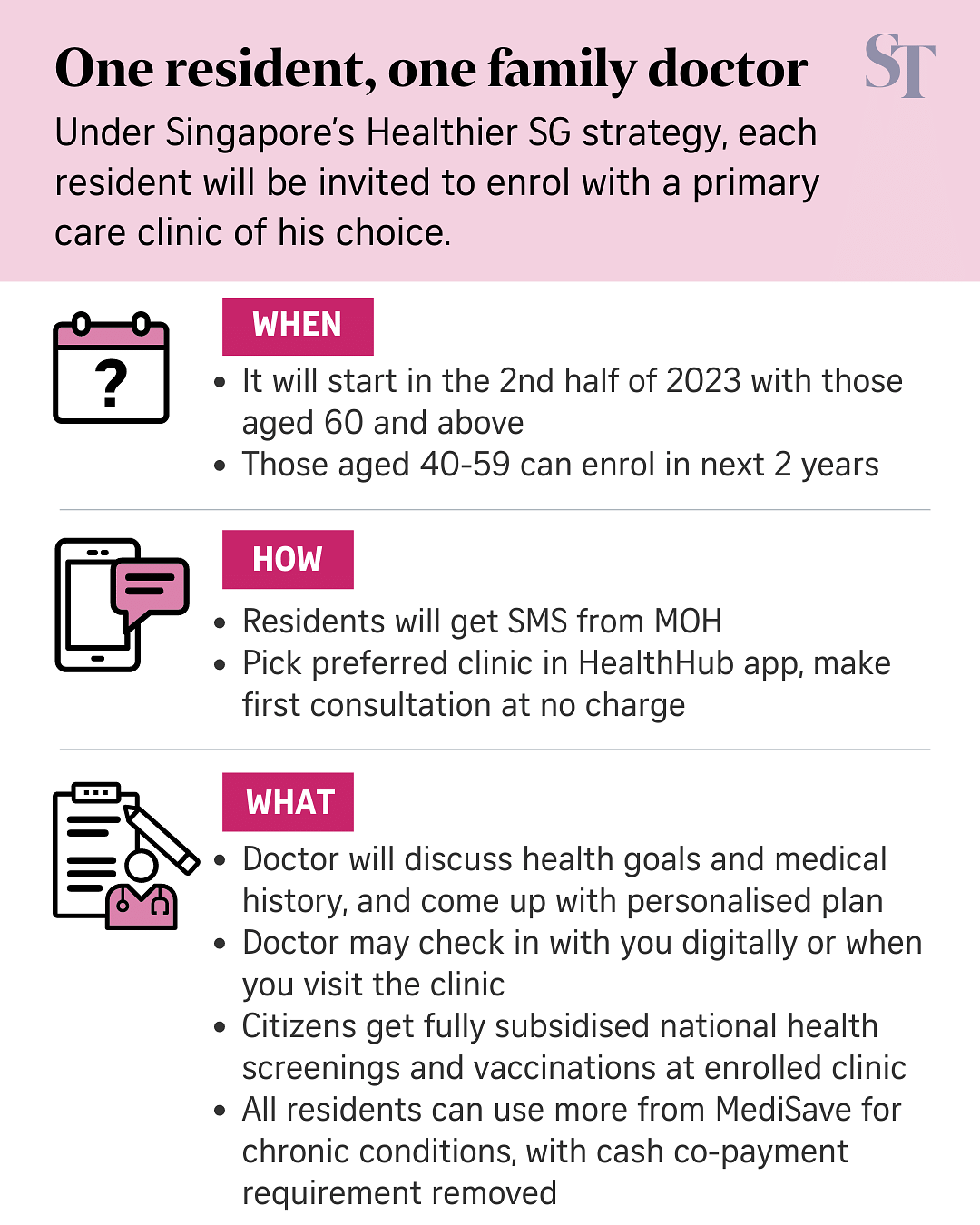
Singapore's ambitious plan to have one family physician and one health plan for each and every one of its residents will start with those aged 60 and above in the second half of 2023.
The Healthier SG Programme will also offer cheaper drugs for chronic diseases at general practitioner (GP) clinics, among other benefits. With it, MOH aims to shift its focus from "sick care" to preventive care so as to eventually help every resident stay on the path to better health.
Eligible residents will be invited to enrol in the programme with a primary care clinic of their choice via SMS. Those in the 40 to 59 age group will be invited to enrol in the following two years, the Ministry of Health (MOH) said in a White Paper that was submitted to Parliament on Wednesday. The White Paper will be debated in Parliament in October.
Since March, the ministry has engaged more than 6,000 residents and other stakeholders for their views on the strategy.
Under the Healthier SG Programme, residents will develop a relationship with a primary care doctor who will holistically manage their health.
At the first visit, which will be free, the doctor will work out a health plan that can include diet adjustments, an exercise regimen and regular health screenings and vaccinations.
Health Minister Ong Ye Kung told the media at the MOH headquarters in College Road on Wednesday that the plan has social prescriptions like "how you eat, how you sleep, how you cut down on salt and sugar, quit smoking, exercise, so on and so forth".
Community partners will be roped in to help manage residents' health, as the idea is to move healthcare away from acute hospitals to the community to help keep people healthy. Residents will be able to join free programmes to keep fit, for instance.
A key change that MOH will introduce to get residents on the programme is to make drug prices at participating GP clinics more comparable with those at polyclinics through a combination of enhanced drug subsidies and drug price limits. This will be done for drugs used to manage common chronic diseases.
With this, people will no longer have to end their relationship with their long-time GPs when they develop diabetes or hypertension just because the drugs for these conditions are cheaper at polyclinics.
MOH will announce the details for this at a later date.
The ministry also said that it will fully subsidise nationally recommended screenings and vaccinations for Singapore citizens, and waive the need for residents to co-pay 15 per cent of their bills in cash when using MediSave for the treatment of common chronic conditions under the Chronic Disease Management Programme.
"We are shifting away from co-payment for this basic preventive care to fully support residents (in) preventive care," said Mr Ong.
There will be a health points reward system to get people to take action, such as to enrol and complete their first consultation, and engage in health activities.
However, to get Healthier SG off the ground, MOH will first have to mobilise family doctors in private practice.
MOH will offer GPs an annual service fee for each enrolled resident, which will vary according to the risk profile, scope of care and the progress made, as well as a tech support grant.
These doctors will need to join a so-called Primary Care Network, partner a healthcare cluster, and be digitally enabled. The Primary Care Networks, which hire nurses and coordinators for chronic disease management and other shared tasks, will support the GPs in their work. There are currently 23 polyclinics and about 1,800 GP clinics, of which 670 clinics have formed such networks.
To ensure the level of care is consistent across GPs, MOH is developing a set of care protocols with primary care leaders to guide family doctors on how to manage key chronic conditions.
Healthier SG will start with the care protocols of three of the most common chronic conditions: diabetes, hypertension and lipid disorders. In the future, the protocols will expand to cover more conditions and areas such as mental health.
"Everyone involved, including healthcare providers, the Government and residents, will need to do things differently," MOH said in the White Paper.
"Healthier SG is probably the most significant change to the health system since Independence. We have had six decades where we emphasised reactive sick care rather than health promotion," said Associate Professor Jeremy Lim, director of the Leadership Institute for Global Health Transformation at the National University of Singapore's Saw Swee Hock School of Public Health.
The incentives under Healthier SG are created to promote health, rather than healthcare and, for the residents, inertia will be the biggest enemy, he said.
It will take years for such a major transformation of the healthcare system to take off and experts said the start will inevitably be challenging before the results show.
"Healthcare expenditure may rise initially and even more rapidly as we discover more people who have medical problems," said Dr Wong Chiang Yin, a public health specialist in the private sector.
"We must have the tenacity to stomach this and stay the course before the benefits of Healthier SG kick in at a later stage," he added.
The White Paper on Healthier SG can be viewed at www.healthiersg.gov.sg.
- Additional reporting by Lee Li Ying
Get The New Paper on your phone with the free TNP app. Download from the Apple App Store or Google Play Store now


